“I remember talking to a mother, whose child had cancer, who told me that after many months she was finally able to sleep through the night because her child was now receiving morphine at the hospital and had stopped screaming in pain,” recalls Dr Salwa Massad, a Research Manager for the WHO Palestinian National Institute of Public Health – occupied Palestine territory.
Salwa touches upon the dire shortage of cancer and palliative medicines, for children with cancer living in the Gaza Strip. Years of conflict and the ongoing siege of the Gaza Strip since 2012 has exacerbated gaps in childhood cancer service delivery, created shortages in cancer medicines, and delayed access to life-saving services such as radiotherapy for children living with cancer.
In 2021–2022, Salwa and the team conducted an assessment of structural barriers to paediatric cancer services in Gaza in partnership with the Ministry of Health (MoH) and WHO. A key early strategy was to involve the MoH closely in the design and roll-out of the survey so as to secure Government buy-in for suggested interventions thereafter. Another strategy was to involve multiple stakeholders in the qualitative study including parents of children with cancer, oncologists, nurses, social workers in oncology hospitals in Gaza and in referral hospitals in the West Bank, MoH focal points, and pharmacists – to gain a better understanding of the scope of the problem and design long-term solutions.
Generating political will and advancing implementation through advocacy
The occupied Palestine territory is one of 67 countries where governments have committed to increase access and quality of care for children with cancer through the implementation of the WHO-St Jude-led Global Initiative for Childhood Cancer (GICC) CureAll Framework. GICC aims to increase the survival rate of children with cancer globally to at least 60% by 2030. Salwa and the team used evidence-based data generated through the survey to make progress towards evidence-based interventions in the two oncology hospitals in Gaza (the Rantisi and the Turkish Palestinian Friendship hospitals) that directly contribute to strengthening paediatric oncology services in Gaza.
Data from the study and the interviews with the mothers of child cancer patients were instrumental in enabling three key achievements:
1) Policy changes in paediatric oncology. Leveraging the voices of children with cancer and their parents, Salwa and her team demonstrated the challenges associated with the age limit (12 years) for transferring children with cancer from Rantisi paediatric hospital to the adult oncology ward of the Turkish-Palestinian Friendship Hospital. She states, “We took the testimonies of oncologists and mothers of children with cancer to Dr Yousef Abu Alreish, the Deputy Minister of Health in Gaza and explained how disruptive the age limit was to their treatment process. We used evidence from published studies to show how outcomes improved when children were kept in paediatric wards.” As a result of these efforts, the Ministry of Health issued policy changes that raised the age limit of paediatric cancer.
Under the Global Initiative for Childhood Cancer, Salwa’s team also advocated for the establishment of an oncology youth ward in the Turkish-Palestinian Friendship Hospital that allowed children to be with others their age as well as their mothers. The wards were designed to enable parents to stay with their children during the course of treatment, an option that wasn’t previously available. Additionally, through the Initiative, a resource room was set up for children who otherwise would spend all day looking at the ceiling for want of any other form of entertainment. The resource room now offers toys, books, activities, and a smart TV to keep children engaged.
2) Promoting early detection and timely referrals. Through the survey, WHO determined significant gaps in early detection and timely referrals among Gaza-based healthcare workers. A cancer oncologist in Gaza described how he hadn’t received any training for over 15 years. Some parents and oncologists shared horrific stories of late/inaccurate diagnosis for children with cancer, partly due to absent or insufficient diagnostic tools. As a result of these testimonies, the Deputy Minister of Health formed a task force to follow-up on reported diagnostic inaccuracies and made provisions for the training of emergency room physicians and paediatricians on childhood cancer early warning signs for timely investigation and diagnosis.
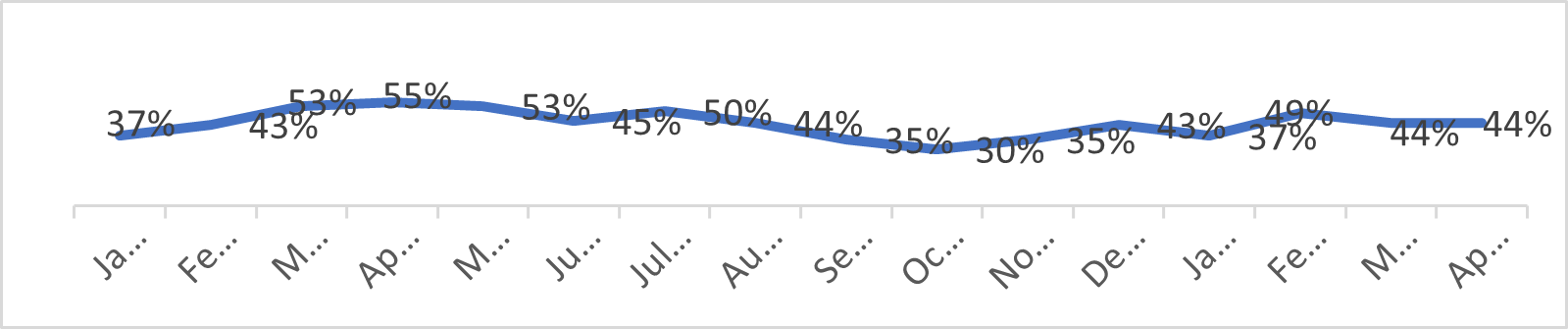
3) Procurement of cancer medicines. Speaking about how difficult it is for children to cope with their illness because of shortages in basic medicines (Figure 1), the head of pharmacists in Gaza who participated in the qualitative study stated: “If we can’t heal children with advanced stages of cancer in Gaza, at least we can help them die with less pain.” Another parent shared how “her son kept screaming all night with pain and the only pain medicine that the hospital could give him was paracetamol.”
Figure 1: Percent of oncology drugs with zero stock at Ministry of Health, by month, Jan 2021–April 2022, Gaza
he Initiative is also preparing to better train health care workers in Gaza to enable early detection of childhood cancers and timely referrals. “All these changes were possible because the Ministry of Health was with us right from day one,” emphasizes Salwa. “We didn’t conduct the study and then go back to them saying ‘this is what you need to implement.’ Instead, we did the study together with them so they had complete ownership over the results.”
Thus, through GICC, the occupied Palestine territory has raised the age limit for transferring children to adult oncology, made provisions for a youth cancer ward, served as a catalyst for the establishment of pain clinics at oncology hospitals in Gaza, and enabled the procurement of palliative care and essential cancer medicines.
Document Sources: World Health Organization (WHO)
Subject: Assistance, Children, Gaza Strip, Health, West Bank
Publication Date: 17/05/2023
URL source: https://www.who.int/news-room/feature-stories/detail/delivering-childhood-cancer-care-in-fragile-and-conflict-settings--best-practices-from-palestine