
World Economic Situation And Prospects: April 2021 Briefing, No. 148
 Adding fuel to the fire? Inequality and the spread of COVID-19
Adding fuel to the fire? Inequality and the spread of COVID-19
The World Health Organization officially declared COVID-19 a “pandemic” one year ago. Since then, the virus has spread like wildfire, upending social and economic life and causing an enormous—and still rising—human toll. As of 19 March 2021, the COVID-19 pandemic had infected more than 122 million people and killed about 2.7 million worldwide. Furthermore, while the vaccination campaigns gain pace globally—more than 400 million single doses have already been administered—the prospects to bring the pandemic to an end and achieve herd immunity are still uncertain. Virus mutations, pandemic fatigue and the uneven global distribution of vaccine supplies pose significant risks to the pandemic trajectory in the coming months.
So far, countries around the world have experienced widely different health impacts from the pandemic. By 10 March 2021, Brazil, Spain, United Kingdom and United States had more than 125 deaths per 100,000 people, while Japan, Ethiopia and Malaysia had fewer than 7 deaths per 100,000 people. There are several factors that help explain the significant differences in infection and mortality rates, including geographical location, population age structure, share of urban population, preparedness of healthcare systems and prevalence of comorbidities and underlying health conditions. The soundness of government responses and the stringency of social distancing measures that have been implemented have also played a major role in containing, or accelerating, the spread of the virus.
This April Monthly Briefing discusses the role that inequalities can have as a catalyzer in speeding up the transmission of the virus. There are several channels through which inequalities are linked to the spread of the COVID-19 pandemic. For example, inequalities are associated with worse population health conditions across countries, which make for a more fertile ground for an infectious disease. Inequalities are also correlated with poverty and deficient access to goods and services that are essential in preventing infectious diseases, such as sanitation, housing and healthcare. Moreover, lack of access to essential goods and services are a factor behind the prevalence of diseases and comorbidities in more disadvantaged groups, further contributing to an unequal burden of morbidity. For example, lower household incomes are associated with a higher incidence of diabetes and heart disease. Even among developed countries there are enormous disparities in healthcare access. In the United States, for example, about 8 per cent of the population (26 million people) did not have health insurance in 2019, making them less likely to seek medical care or to access preventive healthcare.
In addition, inequalities influence social distancing practices, as poorer households are less capable of observing physical distancing and ensuring the effective implementation of lockdowns. In fact, the cost of greater social distancing is much higher for members of poorer families who cannot isolate and continue to work, maintaining their income and levels of consumption. Elevated inequalities are also correlated with lower levels of trust and social cohesion, which can fuel doubts over official health information. Ultimately, lower confidence in public institutions can undermine the compliance with mandatory social distancing and health measures.
There are several prominent examples of countries with relatively high levels of inequality that have been battered by the COVID-19 pandemic. In the developed world, the United States has suffered severe impacts from the pandemic, with one of the highest number of deaths per 100,000 people. Among developing countries, noticeable examples are Brazil, Mexico and South Africa which rank among those with high income inequalities. As of 10 March 2021, these four countries with high levels of inequality accounted for 38 per cent of the global death toll but only 9 per cent of the global population. Some countries with moderate or high income inequality were, however, able to manage and contain the impact of the pandemic. For example, several countries with high income inequality in Africa have largely escaped the virus. To some extent, this can be attributed to their relatively low levels of integration with the world economy. In addition, China—with a relatively moderate Palma ratio of 1.7—imposed strict measures early on, including lockdowns, massive testing and contact tracing, limiting the spread of the virus.
Table 1 provides aggregate information regarding the dynamics of COVID-19 cases and related deaths per 100,000 people and income inequality measures (Palma ratio and Gini coefficient3) for countries with available data. By June 2020, only a few months into the pandemic outbreak, the average number of cases per 100,000 people for countries with relatively low inequality (Palma ratio below 1.5) was similar to the number of cases for countries with relatively high inequality (Palma ratio above 2.1). In October 2020, once the virus had spread more widely, more unequal countries displayed higher numbers of cases—above 600—while countries with lower levels of income inequality had less than 460 cases. This suggests a positive correlation between the number of cases and income inequality (figure 1). Using data for October 2020, a similar picture is observed for the number of deaths.
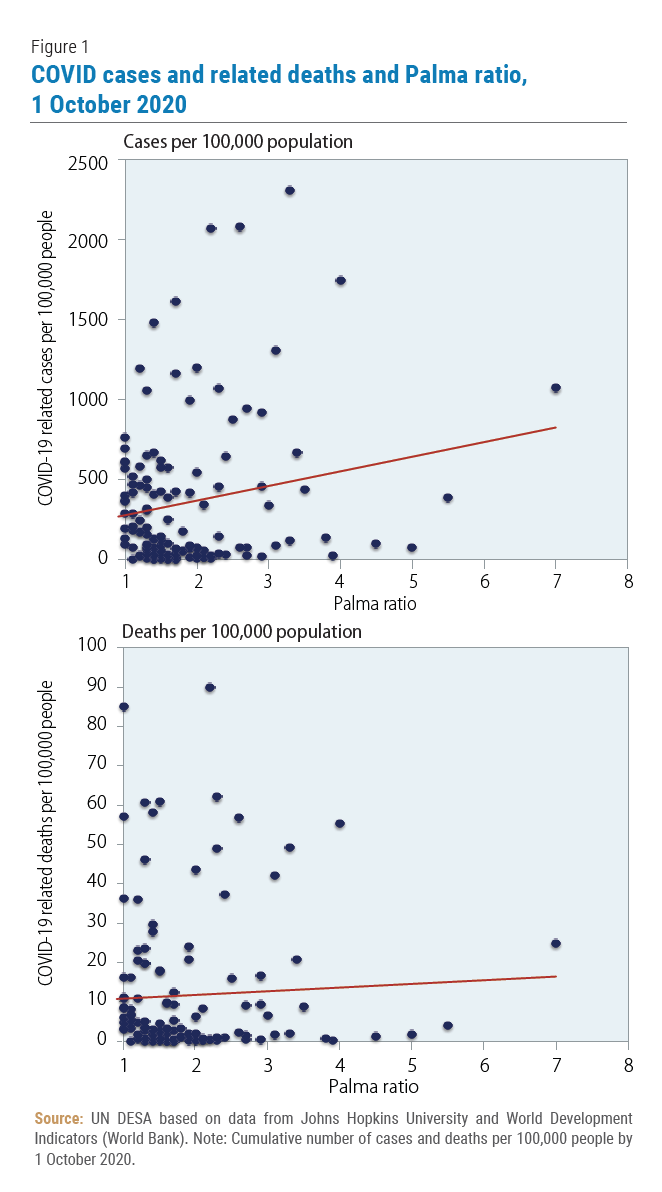 More recent data, however, show that the higher number of cases and deaths for more unequal countries in October 2020 is reversed. With data until March 2021, countries with relatively low levels of inequality had significantly higher numbers of cases and deaths, on average, in comparison to more unequal countries. This comes as major infection waves materialized in the last months of 2020 and the first months of 2021, in countries with relatively low income inequality, such as Denmark, Estonia, Malaysia, Norway, Slovenia and Uruguay. In some countries, the premature loosening of social distancing measures contributed to the upsurge in infections. Similar patterns are observed when using the Gini coefficient as a measure for inequality. This statistical information provides only a partial picture of the relationship between income inequality and the spread of COVID-19 across countries. The income inequality categories in Table 1 are somewhat arbitrary and there is significant variation in cases and deaths within each category, underscoring the need to consider other country-specific factors, such as geographical location, testing capacity and the share of urban population. Notably, the stringency of social distancing measures implemented to contain the pandemic has played a crucial role in curbing the infection rates. The next section discusses a more comprehensive empirical approach to analyze the relationship between inequality and the spread of the COVID-19 pandemic.
More recent data, however, show that the higher number of cases and deaths for more unequal countries in October 2020 is reversed. With data until March 2021, countries with relatively low levels of inequality had significantly higher numbers of cases and deaths, on average, in comparison to more unequal countries. This comes as major infection waves materialized in the last months of 2020 and the first months of 2021, in countries with relatively low income inequality, such as Denmark, Estonia, Malaysia, Norway, Slovenia and Uruguay. In some countries, the premature loosening of social distancing measures contributed to the upsurge in infections. Similar patterns are observed when using the Gini coefficient as a measure for inequality. This statistical information provides only a partial picture of the relationship between income inequality and the spread of COVID-19 across countries. The income inequality categories in Table 1 are somewhat arbitrary and there is significant variation in cases and deaths within each category, underscoring the need to consider other country-specific factors, such as geographical location, testing capacity and the share of urban population. Notably, the stringency of social distancing measures implemented to contain the pandemic has played a crucial role in curbing the infection rates. The next section discusses a more comprehensive empirical approach to analyze the relationship between inequality and the spread of the COVID-19 pandemic.
Adding fuel to the fire?
Disentangling the impact of inequality on the spread of COVID-19 is a complex task. A preliminary UN DESA empirical study attempts to shed light on the relationship by using monthly data on cases and deaths in the first seven months since the first case in each country. In doing so, it specifies empirical equations where the dependent variables are the monthly number of cases and deaths per 100,000 people. As explanatory variables, the estimations use different inequality measures (Palma ratio, Gini coefficient and income share of highest 10 per cent earners), along with several control variables. The empirical approach takes into account the dynamic of the spread of the virus, the different testing capacities and the geographical location of each country. In addition, it controls for other important factors that can affect the spread of the COVID-19 pandemic, including the share of population living in poverty, the share of urban population, the share of population over 65 years and the quality of healthcare systems, among others.
Most importantly, the empirical analysis considers the stringency of social distancing measures implemented in each country and month to curb infections. For this, it uses the stringency variable from the Oxford COVID-19 Government Response Tracker, which measures the degree of intensity of the adopted measures, including school closures, restrictions on gatherings and stay-at-home orders, among others. The implementation of these measures has varied widely across countries. A simple analysis shows that, in the first seven months of the pandemic, more unequal countries tended, on average, to implement more stringent social distancing measures.
The results from the econometric estimations uncover a specific role for income inequality in the spread of the virus. Income inequality is positively and significantly correlated with the number of cases, while the correlation with the number of deaths is somewhat weaker. Also, the results show that the effect of social distancing measures on the number of cases critically depends on the levels of inequality. In fact, social distancing measures are less effective in reducing the number of cases in countries with high inequalities. As such, more unequal countries will likely need more robust public responses to contain the spread of the virus. It is not surprising, then, that more unequal countries have actually tended to be more proactive in the implementation of such measures, on average.
While the econometric regressions do not test for specific channels behind the connection between income inequality and the spread of the virus, working conditions, social distancing and social cohesion are likely to have played a major role. In fact, the diverse working conditions and social distancing possibilities have been an important determinant of how different population groups have been affected by the virus. In addition, the lack of social cohesion provides a causal link between the lower responsiveness of cases to social distancing measures in more unequal countries. More unequal societies tend to have lower levels of trust and social cohesion, which can fuel doubts over official health information and undermine the compliance with mandatory social distancing and health measures. Previous studies related to other influenza pandemics, for example, have shown that protective behaviors—such as wearing a face mask, washing hands and intentions to receive a vaccine—are connected to the confidence in health authorities and social cohesion.
In sum, this research confirms that high levels of inequality mattered in the spread of the COVID-19 pandemic. Inequalities seem to accelerate the transmission of the virus and contribute to a higher number of cases, which indirectly increased mortality rates. It also shows that higher income inequalities reduce the responsiveness of the infection rates with respect to the social distancing measures. Thus, elevated inequalities place societies in a more vulnerable position to confront the pandemic. Fighting high and rising inequality will be critical for reducing vulnerability to health and other emergencies and for enhancing the resilience of societies in the years to come, not least as an indispensable step towards sustainable development. As United Nations Secretary-General António Guterres put it recently, “Inequality defines our time (…) Now is the time for global leaders to decide: Will we succumb to chaos, division and inequality? Or will we right the wrongs of the past and move forward together, for the good of all?”


Follow Us