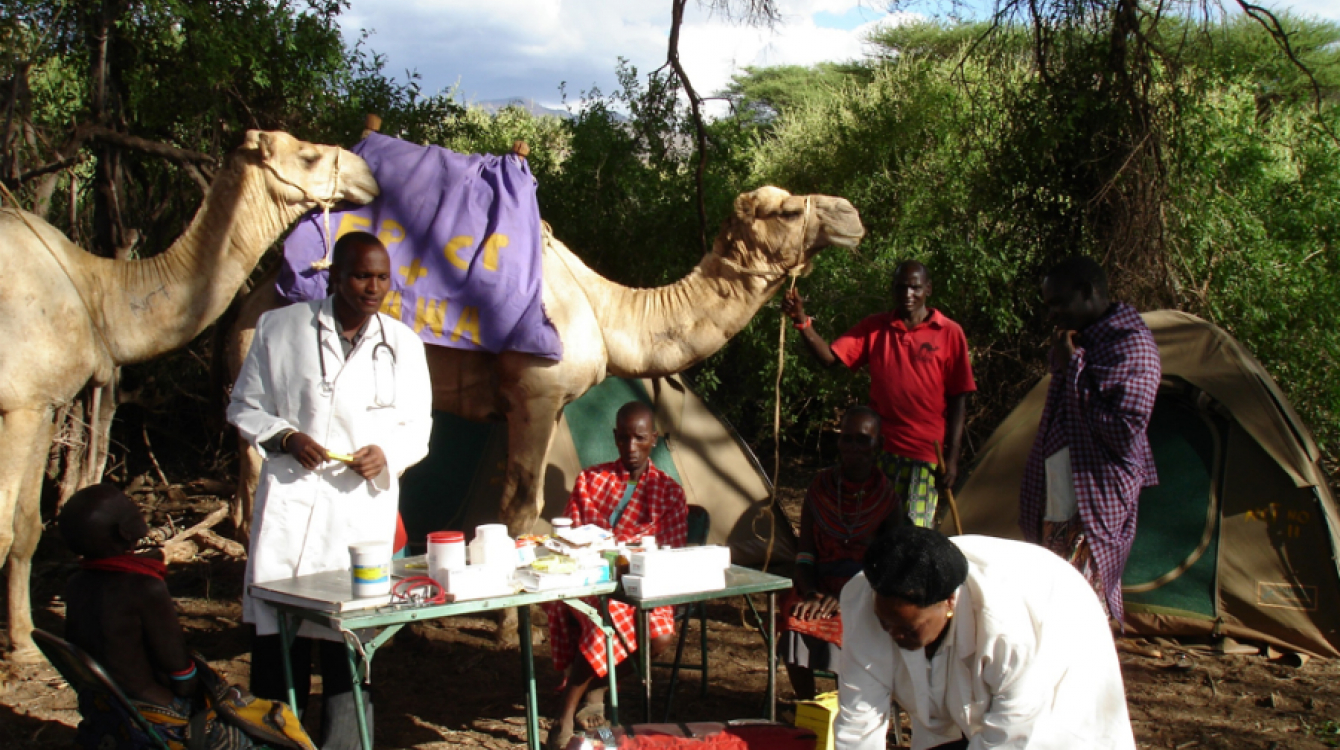
Taking health services to remote areas
Taking health services to remote areas
The camel is known for its resilience. Carrying heavy loads in sweltering desert heat over 160 km with little water to drink is no easy job.
This “ship of the desert,” however, is built for such terrain—thick footpads help it navigate shifting sand and rocky paths with ease; long legs keep its body away from the surface heat; closing nostrils keep sand at bay; and bushy eyebrows and eyelashes protect the eyes.
These adaptive characteristics and physical features have come in handy for a novel transport system that ferries medical supplies and personnel to remote villages and underserved communities in Kenya.
In neighbouring Uganda, motorcycles are the alternative transport of choice, bringing health care to the remotest areas, while in Malawi, mobile phone technology is being used to combat maternal deaths.
Camel clinics
In Kenya’s Samburu County, with harsh climatic conditions and more than 50% of the population living below the poverty line without adequate sanitation, many may die in childbirth or from treatable diseases such as malaria, diarrhoea, tetanus, waterborne diseases and eye and skin infections.
To reach the residents in this remote county, which is more than 300 km north of the capital, Nairobi, camel mobile clinics now traverse the vast area whose terrain is thorny scrubland and semi-arid bush.
Camel mobile clinics have been hailed as one of the more innovative and sustainable means of reaching local communities in far-flung areas. An initiative of Communities Health Africa Trust (CHAT), a non-governmental organization started 16 years ago by Shanni Wreford-Smith, the camel mobile clinics were started six years later and they target these semi-nomadic communities that move from place to place in search of pasture and water.
According to Ms. Wreford-Smith, a mobile clinic comprises 7 to 10 camels, a team of medical workers and camel handlers. In the group are also two family planning and HIV counsellors.
“A normal day for our camel clinics entails waking up early to pack and load the medical supplies on the camels and start the journey before the sun gets too hot. The team walks at the pace of loaded camels and sometimes a distance of 25 km can take a whole day to cover, sometimes we take between two to six hours,” Ms. Wreford-Smith told Africa Renewal.
Once at their destination, the convoy pitches tent near a big manyatta (a traditional homestead established by a family or clan) for two to three days while members of the team do door-to-door mobilizing. The clinic serves on average 30 to 80 people, depending on the size of the manyatta, before moving on to the next group. It provides basic health services and holistic family planning, “integrating a strong component of ecological awareness and sensitization.”
“We target communities in dire need of health services for common diseases such as malaria and diarrhoea,” says Violet Otieno, a social worker and project officer at CHAT. The clinics also do HIV/AIDS testing and counselling, and referrals for antiretroviral treatment.
The camel mobile clinics are donor-funded, which limits the number of trips they make to at least four circuits per year—with each circuit taking up to two weeks.
The team has learned to safely navigate various risks, including dehydration, attacks from wild animals and being caught between warring clans. It has lost only four camels to sickness since the clinics started 10 years ago.
“The good thing is that the camels enable us to reach places where vehicles cannot [go],” Otieno says, adding that CHAT has now expanded the camel mobile clinics to other counties, including arid and semi-arid Isiolo, Marsabit, Molo and Kitui, to serve these marginalized communities.
In Samburu, like other vast areas in northern Kenya that are inaccessible due to nearly impassable roads, locals are forced to walk for hours to obtain urgent medical care. This has made the camel mobile clinics the most convenient means of providing health services.
In one Samburu village, 34-year-old Jeremiah Samana struggled to contain his tears as he recounted the moment he watched his wife’s life ebb away while she was giving birth to their third child. “If it were today [with the camel mobile clinics], she would be alive,” he told Africa Renewal.
Today, as Samana watches camels loaded with medicines plod past his manyatta to deliver services to his neighbours, he is grateful that, although they came a little late to save his wife, he and his children are beneficiaries of the services.
Motorbike ambulances
Health services are hard to come by in Turkana, Kenya’s largest county. A shortage of health personnel means that one doctor serves about 50,000 people. The new county government has devised ways of taking health services nearer to the people in this vast, rural county.
“We use motorcycle ambulances to reach our people in the county’s seven sub-counties. Since the introduction of this innovation, many people can easily access health services,” Jane Ajele, the county’s health minister, told Africa Renewal.
The ministry has six motorcycle ambulances serving the sub-counties. Demand for the services is high, and Ajele says there are plans to increase the number before the end of this year.
“The good thing about these ‘ambulances’ is that they can navigate impassable roads to save lives. Besides carrying medicine, they also ferry women in labour to the nearest health facility,” she said.
Similarly, Tana River County has introduced four motorcycle ambulances for piloting in four remote villages which have one of the highest numbers of maternal deaths in the country. The villages are Biressa, Dende, Wayu-Boro, and Tawakal.
Uganda’s village ambulances
As of last June, Uganda was using motorcycle ambulances to reach people in the rural western region.
Commonly known as “village ambulances,” these three-wheeled motorcycles take medicines, medical supplies and information to patients in remote villages. Before their introduction, community health workers would use improvised stretchers, or carry the sick on their backs to the nearest health facility. Many never made it, as the journey was long and arduous.
“With the village ambulances,” Swizen Kisembe, a health worker, told the South African Broadcasting Corporation in September, “many lives are being saved.”
Village ambulances have also turned out to be cheaper and safer than conventional ambulances.
Malawi: Health e-Innovation
Malawi’s “health centres by phone” have discovered a novel way of providing crucial health care services to people in rural areas through the use of text messages.
A basic phone becomes a clinic through which a patient gets all the information he or she requires from a doctor without going to a clinic. The text message service also gives tips and reminders about taking medications, making it easy and convenient to connect patients and health providers any time of the day.
This has proven helpful in providing pregnant women with necessary prenatal and also postnatal information. Some of the messages encourage the use of mosquito nets to prevent malaria, others give tips for preventing mother-to-child HIV transmission and for improved health care in general.
The toll-free line, supported by Airtel, a mobile phone company, serves more than 500,000 mothers and children. The Malawi government, which aims to reduce maternal mortality, has endorsed the mobile phone innovation.